How Much Iron Do You Need During Pregnancy? + 8 Facts About Getting Enough Iron Pregnant Women Need to Know
TL;DR

Iron during pregnancy is one of the most popular topics I consistently address via email and DM.
And with good reason!
Iron is a critical mineral needed for growth and development. Iron levels should be monitored and adjusted while trying to conceive and during pregnancy. Many aspects of you and your developing baby’s health depend on it.
That said, the number one question I receive has to do with the fact that FullWell Women’s Prenatal, well, doesn't contain any iron.
Our Women’s Prenatal does not have iron in it by design. Let me explain.
Iron needs and tolerances vary significantly by individual. The amount of iron your body requires changes as pregnancy progresses, and getting enough iron is critical for health at every stage.
However, not all women need to supplement with iron to keep their levels in an ideal range.
Plenty of women get enough iron through diet alone (which makes me - the real food dietitian - extremely happy! More on that later).
For those who need to supplement, matching the form and dose of iron to individualized, specific needs may be best. In my experience, I’ve learned that monitoring your iron status during pregnancy with your healthcare practitioner will always be your best bet, as form and dosage are much more unique to each individual.
This way, if you need supplemental iron, you’ll know which form to take and consume it separately in appropriate doses at your healthcare practitioner’s recommendation.
This will help avoid unnecessary digestive distress, avoid interfering with the absorption of other vital nutrients, and keep you from consuming too much or too little iron overall.
So, in short, I didn’t leave iron out of our Women’s Prenatal because it’s unimportant. I left it out because it’s so important that it should be tended to on its own, apart from your (equally important) comprehensive prenatal multivitamin.
Iron is such a big deal that it gets its own blog post! Read on to learn more about:
- What is Iron, and Why is It So Important?
- How Much Iron Do Pregnant Women Need?
- What are the Best Iron-Rich Foods for Pregnant Women?
- Am I At Risk for Iron Deficiency During Pregnancy?
- Why is Iron Essential Before, During, and After Pregnancy?
- Will My Iron Needs Change Once I Become Pregnant?
- How Do You Address Iron Concerns in Your Private Practice?
- Which Labs Do I Need to Ask For to Assess My Iron Levels Accurately?
- If I Have to Take Iron Supplements During Pregnancy, What are the Best Ways to Go About Finding the Right One?
We’ve got a lot to cover, so let’s start at the very beginning.
1. What is Iron, and Why is It So Important?
A basic, general understanding of the importance of iron in the human body dates back to ancient times (1).
Some evidence suggests advanced civilizations such as the Egyptians, Hindus, Greeks, and Romans used iron for medicinal purposes to treat symptoms that resulted from (or resembled a result of) iron deficiency.
Not bad, early science!
But don’t worry: the research we base our current recommendations and further exploration on did not begin until the mid-twentieth century. As you’ll see in this post, it is still ongoing and constantly updated.
Today, we know that iron is a mineral that your body needs for cell growth and development (2). The types of iron found in your body may be referred to as elemental iron.
Most importantly, iron is used to create:
- Hemoglobin: a protein found in red blood cells that carries oxygen from your lungs to the rest of your body
- Myoglobin: a protein that provides oxygen to muscles
Your body takes iron from food through the small intestine and uses a protein called transferrin to distribute it.
About 70% of that iron helps create hemoglobin in your blood and muscles, which carries oxygen throughout your body (3).
The rest is mostly ferritin, which we like to think of as a storage container for iron.
It acts as a warehouse within your cells, where extra iron is safely stored when not immediately needed. This helps prevent iron overload and protects your organs from potential damage caused by excessive iron levels.
The average non-pregnant adult woman has about 300 milligrams of stored iron in her body (which, in context, is enough to last for about six months).
2. How Much Iron Do Pregnant Women Need?
Now, not all of us fall into that “average” category.
The National Institutes of Health recommends roughly 18 mg of iron per day for non-pregnant women and 27 mg of iron per day for pregnant women (2).
Even before pregnancy, deficiency is not uncommon for various reasons, including diet. Many women adhere to specific diets that, by nature, lack sufficient iron, putting them at a much greater risk for iron deficiency.
I’ve already hinted at it (and will repeat it before the end of this post), but the best way to ensure your iron intake is adequate is through food.
Learn more about the FullWell Iron Bump supplement and how it can help support your iron intake.
3. What are the Best Iron-Rich Foods for Pregnant Women?
I discuss this term quite a bit regarding supplements, but it also applies to real food: bioavailability matters.
Remember, all I mean when I use the term “bioavailable” is how well your body absorbs and utilizes a nutrient.
- High bioavailability = easily/quickly absorbed
- Low bioavailability = not as efficiently absorbed
There are two types of iron you can acquire through diet:
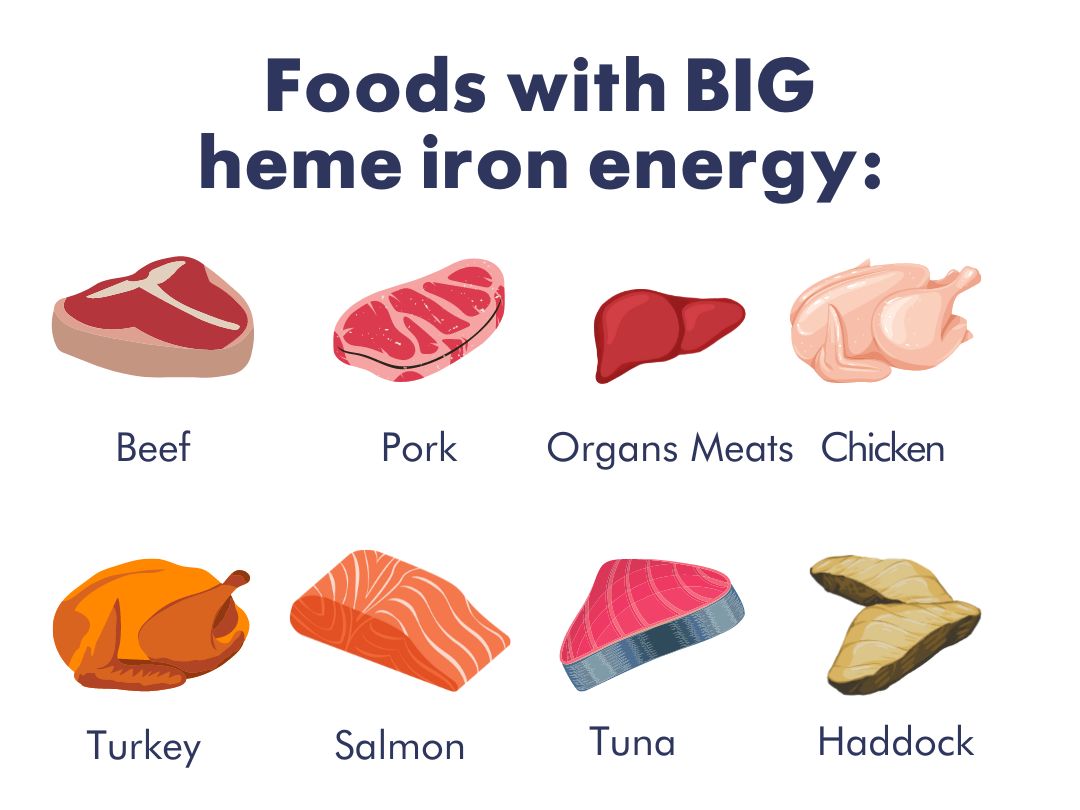
- Heme iron: found in high quantities in animal proteins and is highly bioavailable (about 25-40%)
- Nonheme iron: found in plants, holds a much lower absorption rate (2-13%). Non-heme iron is more challenging for your body to absorb, which means it also physically takes longer before your body can put it to work
For women who eat animal products and byproducts as their sources of iron, getting the proper amount of iron in your diet alone is quite doable. The foods richest in iron are staples in a Western diet.
For vegan and vegetarian women, however, it’s a bit trickier.
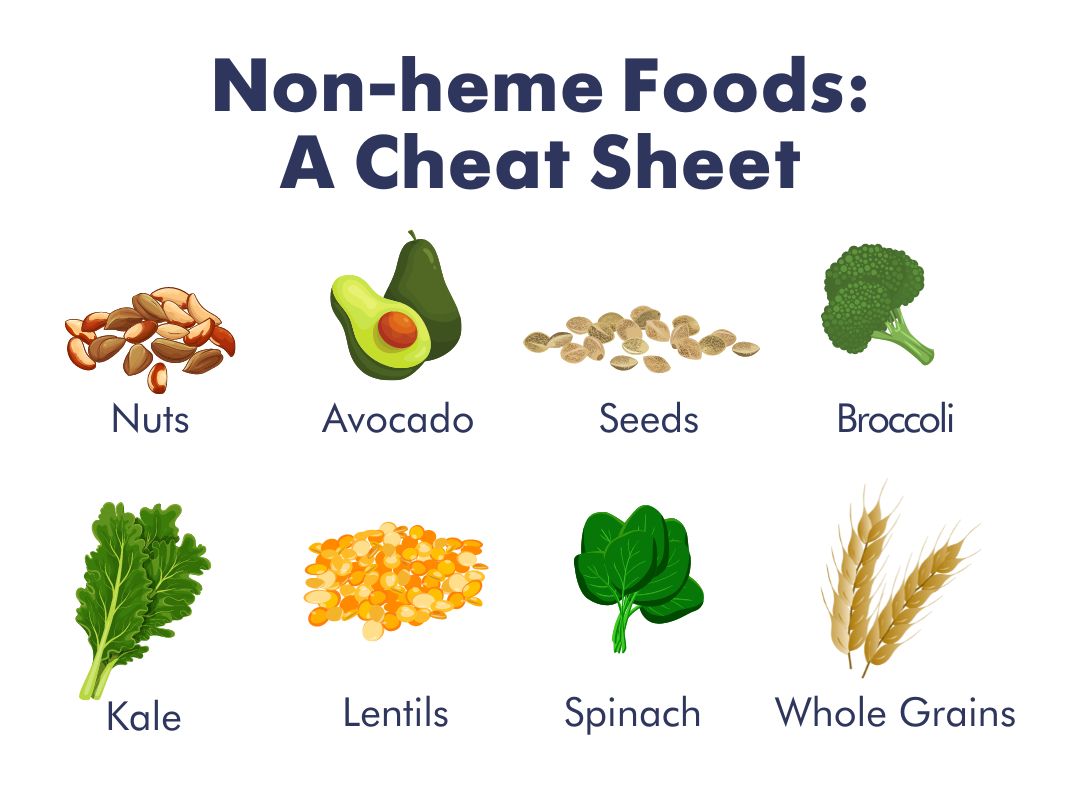
Many plant-based whole foods contain iron, but remember, these will all be in the nonheme form.
When it comes down to animals vs. plants, the issue lies with bioavailability.
To get the amount of iron you need even before pregnancy without consuming meat, you’d have to eat truly enormous volumes of these foods even to have a shot at absorbing enough iron.
And while many foods, like cereals, are fortified with iron, this iron is absorbed poorly, which often leads to digestive discomfort, which we are trying to avoid at all costs (4)!
One thing that can help plant-sourced nonheme iron become more bioavailable is to eat it with another food that is high in vitamin C (e.g., bell peppers, citrus, strawberries, tomatoes, etc.) (5).
For iron to be absorbed properly, it needs an acidic environment in the gastrointestinal tract.
Vitamin C helps create this environment.
However, it is also important to note that any vitamin C-rich foods fortified with calcium (like many orange juices) should be avoided while pairing your food, as calcium inhibits iron absorption (6).
There are a handful of additional compounds that can also inhibit the absorption of iron (7), including:
- Phytates: found in grains and nuts
- Oxalic acid: which is found in high amounts in spinach and rhubarb
- Polyphenols: specifically polyphenols found in tea, coffee, and chocolate
Plant-based eaters are on my shortlist for people who might need to consider supplementation.
As you read on, you’ll discover how to talk to your healthcare practitioner about thoroughly testing your iron through lab work and decide what kind of supplementation is best for you.
For vegan and vegetarian women, however, it’s a bit trickier. Many plant-based whole foods contain iron, but remember, these will all be in the nonheme form.
4. Am I At Risk for Iron Deficiency During Pregnancy?
Diet aside, iron loss through substantial bleeding (e.g., heavy menstrual periods) is one of the most common causes of iron deficiency in women before they become pregnant.
Significant blood loss can lead to iron deficiency, so if you tend to have intense periods preconception, it might be a sign that you need to increase your iron-rich food intake and consider taking an iron supplement.
Some who suffer from chronic gastrointestinal disorders such as celiac disease or inflammatory bowel disease can also quickly become iron-deficient (and even deficient in a whole host of nutrients) due to decreased absorption through the digestive tract.
This also applies to people who have undergone bariatric procedures, especially gastric bypass operations or gallbladder removal.
While it’s not ideal, mild iron deficiency isn’t scary.
Once you know your needs, there are ample ways to course-correct. Iron deficiency anemia is an underdiagnosed condition you become more susceptible to when your blood lacks ample healthy red blood cells to carry oxygen to your body (8).
You might be suffering from iron deficiency anemia if you experience any of the following symptoms:
- Extreme fatigue and a general feeling of weakness
- Chest pain, erratic heartbeat, shortness of breath
- Headache or dizziness
- Poor appetite
Learn more about FullWell’s Iron Bump supplement here.
5. Why is Iron Essential Before, During, and After Pregnancy?
Preconception
The absolute best time to evaluate your iron status is before you even start trying to conceive so that you can get ahead of the game!
While trying to conceive, you should be aware of your iron intake through food and consider taking additional steps with your doctor if your lab results show room for improvement.
This is the most straightforward stage to fix iron levels while on your pregnancy journey, as the stakes are relatively low (barring you suffering from any symptoms).
Working with your healthcare provider to get your levels within range is the first and most productive step you can take.
While Pregnant
During pregnancy, you need a significantly greater amount of iron than non-pregnant women because the amount of blood in your body is increasing to provide for yourself and your baby (2).
Needs also vary by trimester, so you must have enough to make more blood in your own body that will supply oxygen to your baby as they develop.
This is why starting from a depleted state is not ideal.
Your needs increase so rapidly to begin providing for Baby that you can quickly run through your stores and still have trouble catching up and getting enough iron during pregnancy, which could lead to iron deficiency anemia.
If untreated, this could increase Mom’s susceptibility to infection and impact energy levels, breastmilk production, and mood.
For babies, Mom’s iron deficiency can affect their iron stores during the first few months of their life, impacting weight and brain development.
Postpartum
Postpartum anemia usually results from:
- Being iron deficient before becoming pregnant;
- Continued inadequate iron intake during pregnancy, and;
- The blood loss experienced during delivery (9)
This triple whammy produces the exact combination of circumstances that lead to postpartum anemia, which can impact mood, stress resiliency, energy levels, and cognition.
6. Will My Iron Needs Change Once I Become Pregnant?
Will they ever!
The physiological iron demand in pregnant women increases throughout pregnancy (10, 11).
Roughly a third of the iron you consume will be put toward Baby’s growth and the placenta.
About half will contribute to red blood cell expansion, and a quarter will be lost in blood during vaginal delivery (even more with a cesarean).
During the third trimester of pregnancy, Baby's growth accelerates rapidly, which is when most of the iron transfer from Mom to Baby occurs (12).
As Baby develops, your needs will change at different stages of pregnancy, and it isn’t always as easy as generally needing more as you go. Getting specific with your doctor will be extremely helpful.
7. How Do You Address Iron Concerns in Your Private Practice?
I look at the big picture first and then dive in deeper to find the root cause of any issues.
Iron can be affected by a lot of different variables, and many things must fall into place before iron can be absorbed.
A healthy digestive system is critical, as are adequate amounts of specific enzymes, hormones, and proteins that bind with and transport nutrients into the bloodstream.
This might surprise you, but stomach acid is essential for iron.
Over-the-counter medications such as antacids and acid blockers can lead to malabsorption, so if you experience any heartburn or reflux, speak with your healthcare practitioner about how to treat it to ensure you maintain your gut health (13).
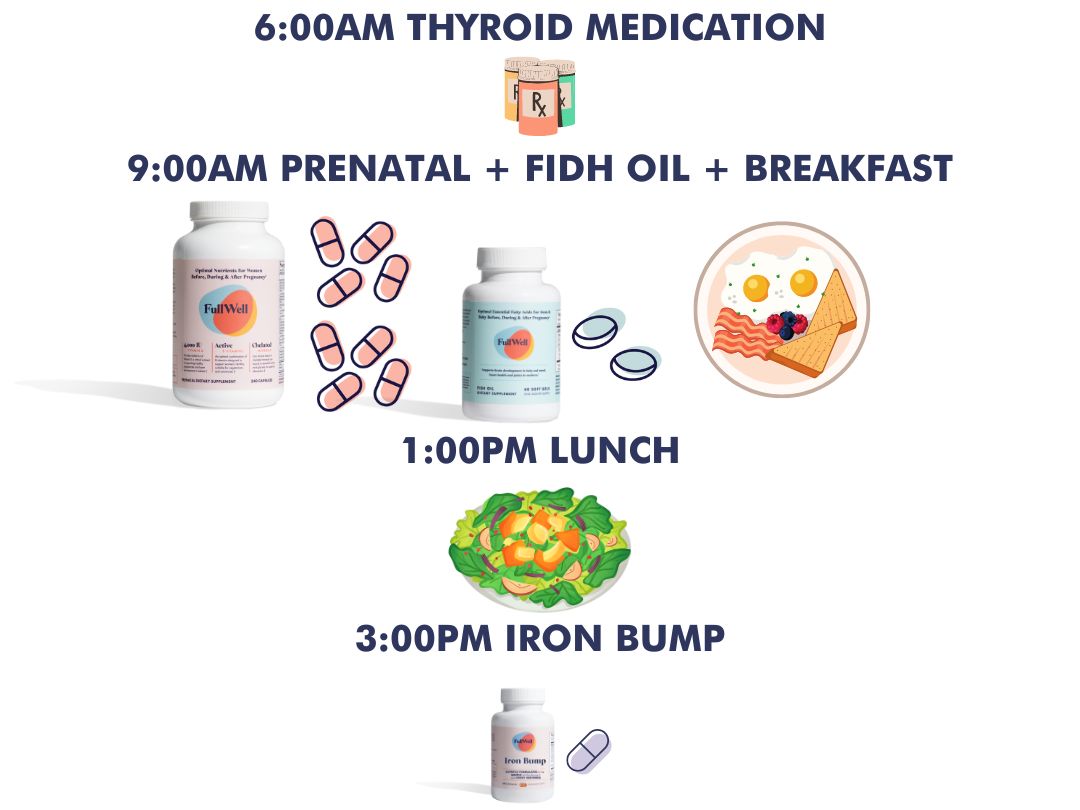
Iron supplementation can also interfere with the absorption of Levothyroxine and other thyroid prescriptions. If you are on thyroid medication, it’s best not to take it within four hours of iron supplements or as prescribed by your endocrinologist.
If I haven’t stressed this enough, let me tell you again...
The best way to ensure you get the iron you need is through your diet.
This means I always thoroughly analyze what foods my private practice clients typically eat and take note of how and when they are eating them to ensure the most iron-rich foods have the best shot at efficient absorption.
Finally, I work with my clients and their healthcare providers to ensure that their labs are ordered and interpreted correctly.
This can be a tricky subject as the labs required to understand how much iron you are absorbing can get confusing, but bear with me. I’m going to lay it all out for you.
This is the part you’ve all been waiting for!
8. Which Labs Do I Need to Ask For to Assess My Iron Levels Accurately?
I love that so many of you ask specific questions about lab work!
Knowing what you don’t know and advocating for yourself by asking questions is such an admirable quality.
I’m preaching to the choir when I tell you that while your doctor is probably fantastic, being informed and involved in lab work never hurts. After all, it’s your body and your baby!
Before I get into specific labs to check your iron levels, let’s explore what we’re looking at/for.
Let’s Talk About Hepcidin.
When we consume and absorb too much iron, it’s not like a water-soluble vitamin, like B12, that we can simply excrete.
Instead, our body employs a safeguard to protect us from overdoing it. Hepcidin, a hormone produced by the liver, acts as a gatekeeper, controlling the movement of iron in and out of cells.
When iron levels are high, hepcidin production increases, reducing iron absorption from food and supplements and limiting the release of stored iron from ferritin. This helps prevent iron overload.
Conversely, when iron levels are low, hepcidin senses it and produces less, allowing more iron to be absorbed from the diet and released from ferritin for us to use.
Ferritin Levels for Pregnancy: Critical Tests for Evaluating Iron Status
Regarding your lab work, ferritin is one of the most sensitive and specific tests for evaluating iron status.
Since ferritin is the primary storage form of iron, it’s the simplest way to catch low iron early. This test is utilized to identify iron deficiency in individuals who do not have inflammation, fatty liver disease, or hyperthyroidism.
Low ferritin is a red flag, but too much isn’t good either. In the presence of inflammatory processes or chronic diseases, ferritin levels can be falsely normal or elevated, despite the presence of anemia.
Checking C-reactive protein (CRP) levels during periods of inflammation can help determine if ferritin is falsely elevated (10). If CRP levels are elevated, consider re-evaluating ferritin once the inflammation has decreased.
A comprehensive iron panel includes the following (14):
- Serum iron test — Measures the concentration of iron in the blood. It provides an overall assessment of iron levels but does not give a complete picture of iron status alone
- Transferrin test — Directly measures the level of transferrin in the blood, which is the protein that transports iron around in the body. This test helps assess iron deficiency and monitor response to treatment
- TIBC (total iron-binding capacity) — measures the total amount of iron that can be bound by proteins in the blood. It indicates the body's capacity to transport iron and is used to evaluate iron deficiency or excess
- Transferrin saturation — A calculation that reflects the percentage of transferrin that is saturated with iron. In cases of iron-deficiency anemia, TSAT levels are typically low. This indicates that a smaller percentage of transferrin is saturated with iron because of inadequate iron availability
- Serum ferritin — Measures the concentration of iron in the blood. It provides an overall assessment of iron levels but does not give a complete picture of iron status alone
- C-reactive protein (CRP) — if ferritin is normal but HgB and HcT are low, this measurement can help determine what role inflammation may be playing
A Note on Iron Deficiency Anemia
Good news and bad news: Iron deficiency anemia comes on gradually.
This is good news because it means once you know whether or not you are deficient, you have time to correct it. It’s bad news because, unless you’ve run your labs, you might not even realize you are at risk.
When your rate of iron loss exceeds the amount of iron you absorb from food or supplement intake, iron stores are slowly used up.
At this stage, ferritin will be low, but serum iron and TIBC will usually look normal while you are still not quite dipping into the anemic range.
As the iron deficiency worsens, serum iron levels fall, TIBC and transferrin rise, and anemia begins to develop.
Then, with prolonged or severe iron deficiency, the red cells become small and pale due to decreased hemoglobin levels, and the other symptoms we’ve discussed might begin to take center stage.
Stay on top of your labs so that you can be well-informed enough to make the right decisions and you will be just fine!
9. If I Have to Take Iron Supplements During Pregnancy, What are the Best Ways to Go About Finding the Right One?
Once your lab results come back, your healthcare practitioner will help you determine what is right for you depending on which stage of your pregnancy you are in or where your lab results fall.
When it comes to iron supplements, there are two key must-haves you should be on the lookout for.
First, Form Matters…
Iron supplements can come in many forms including ferrous sulfate, ferric citrate, ferric sulfate, ferrous gluconate, ferrous bisglycinate, etc.
How do you know where to start? We’ll simplify things for you! There is one form of iron that is not only bioavailable but also associated with fewer digestive side effects: iron bisglycinate.
In most cases, a 25mg daily dose of iron bisglycinate has been shown to be as effective in preventing iron deficiency and iron deficiency anemia in pregnancy as the more common (but more difficult to tolerate) form of iron, ferrous sulfate (15, 16). Iron bisglycinate has also been shown to be a better option than conventionally used iron salts as it has at least two-fold higher bioavailability and absorption with fewer digestive side effects (17).
Second, Look for Ingredients That Help Create the Right Environment for Iron to be Absorbed
For iron to be absorbed properly, it needs an acidic environment in the gastrointestinal tract.
Vitamin C helps create this environment and it is also useful for its ability to bind with non-heme iron from plant sources and transform it into a form that is more easily absorbed (18).
FullWell’s Iron Bump is expertly designed to provide your body with bioavailable iron while avoiding gastrointestinal discomfort.
We use iron bisglycinate, a gentle on-the-stomach and non-constipating form of iron, to ensure optimal tolerance and absorption.
Our innovative formula also contains whole food nutrients, such as vitamin C from acerola cherries, which aid in iron absorption by creating the ideal acidic environment in the GI tract.*
Our ideal 2:1 vitamin C-to-iron ratio increases iron bioavailability, and our proprietary blend further promotes tolerance and digestive comfort (19).*
It’s All About Dosing + Timing
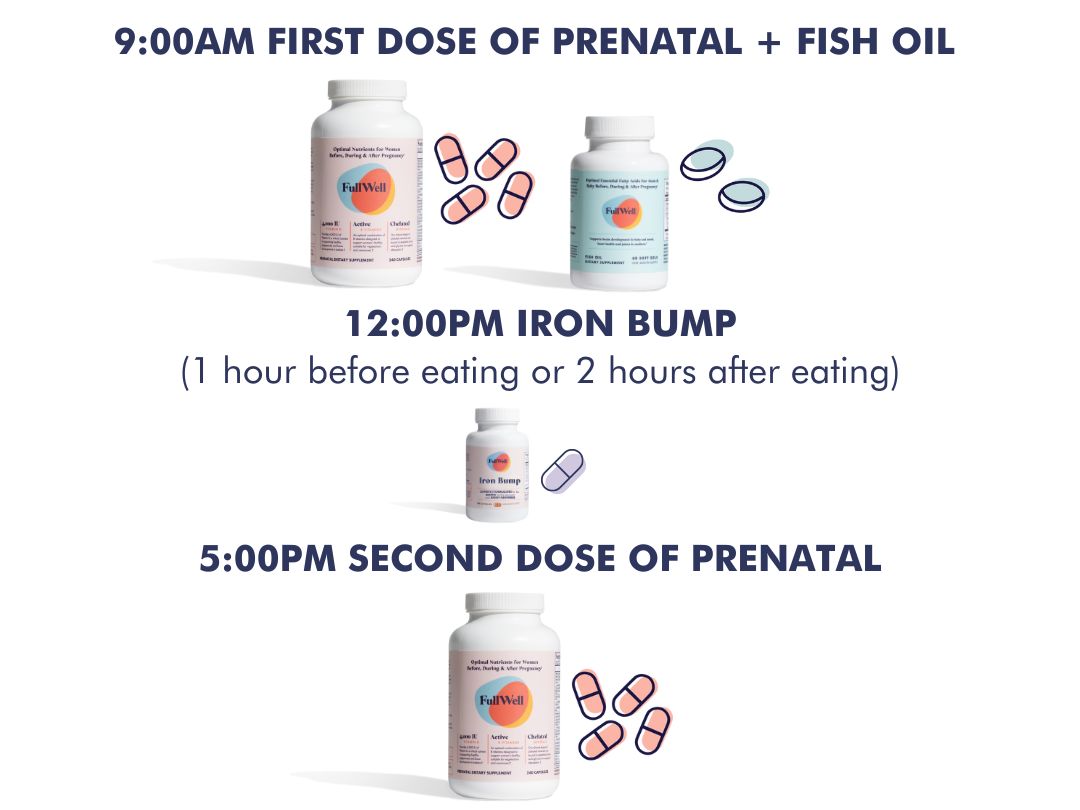
Timing definitely plays into iron absorption.
Iron should be taken on an empty stomach, at least an hour before meals or two hours after to prevent many of the inhibitors of iron found in either foods or drinks from interfering with iron absorption.
The same goes for other supplements you may be taking!
As I mentioned above, calcium can interfere with iron absorption, even in more bioavailable forms, such as dicalcium malate (which is the form of calcium that’s in our Women’s FullWell Prenatal).
I always have my private practice clients stagger prenatal vitamins with iron supplements to allow them more time and a better chance of being digested and absorbed properly for optimal results.
Sometimes women taking high doses of iron supplements on an empty stomach can experience constipation, nausea, abdominal pain, vomiting, and fainting, so if any discomfort does arise, taking it with a meal or snack may be preferable.
Due to the impact of hepcidin on iron absorption, non-pregnant women should take supplemental iron in either the morning or afternoon.
This is when hepcidin is the lowest, which means you’ll have a better chance of absorbing the iron you are taking.
Hepcidin naturally declines during pregnancy, especially during the third trimester.
For athletes or those who are sweating a lot (e.g., high-intensity workouts, resistance exercise, sauna), iron should be consumed three hours before or after training to avoid taking it during a phase of inflammation when hepcidin is highest (20, 21).

Personalize Dose and Timing in 5 Easy Steps
Step 1: Test
Step 2: Determine the dose with your practitioner
Step 3: Set a schedule and consider the following:
- Contraindications
- Drug Interactions
- Exercise
- Other supplements
- Meals
- Alternate day dosing (refers to a dosing regimen in which iron supplements are taken every other day instead of daily. Before deciding to use the alternate-day dosing regimen, it's important to consult with a healthcare professional. This dosing may not be suitable for everyone, and certain factors, such as the severity of iron deficiency, individual tolerance to iron supplements, and specific medical conditions, should be considered. While alternate-day dosing can help manage side effects, it may prolong the time required to achieve optimal iron levels)
Step 4: If you have iron deficiency anemia, work with your practitioner to identify the cause and treat it
Here's a potential sample schedule for someone taking our Iron Bump along with our Women’s Prenatal and Fish Oil:
Here’s another sample schedule for someone taking thyroid medication:
Step 5: Retest!
At a minimum, retest your iron levels 1-2 months after beginning supplementation.
This helps ensure that your anemia or iron lab values are improving and allows treatment to be adjusted as needed.
Remember to communicate with your healthcare provider about whether they’d like you to avoid iron supplements for a certain period before the test, typically 24 to 48 hours, to allow your iron levels to stabilize and provide a more accurate reflection of your iron status.
Have more questions about iron? Reach out to hello@fullwellfertility.com.