3 Ways Postpartum Depression Affects Families
TL;DR
- Postpartum depression can affect every member of the family.
- Mental healthcare is necessary healthcare.
- Learn what to look for in new moms, dads, and siblings and discover how best to support them.

Bringing a new baby home is perhaps one of the most emotional times in our lives.
New moms have a LOT to deal with after having carried and birthed a human being, but the entire family feels all of the roller coaster emotions and physical stressors of adjusting to a new - and very dependent - member of the household.
I know this firsthand.
Despite my extensive background as a functional medicine dietitian focused on fertility, pregnancy, and women’s health, nothing could’ve prepared me - and even my husband - for the postpartum experiences of bringing our first (and then second) child into our lives. It goes to show you that there are some things in life that no one can fully prepare for, even the experts.
Everyone’s experience is unique and valid, and we all deserve support during this very important time.
So in honor of National Depression Screening Day, I’d like to dedicate this post to all of the families working to make it work. Let’s take a look at how postpartum depression affects families on both the micro and macro levels. This way, we can know what to look for, delve into coping and treatment strategies, and destigmatize this very real, very normal occurrence. Mental health care is necessary health care. There is no reason to shy away from it.

1. Let’s start with what seems obvious: mothers (and often first time mothers) are at risk for experiencing varying degrees of postpartum depression, especially if they already have a history of depression, anxiety, and other mood disorders.
50-75% of women experience “baby blues”. 15% of those women experience postpartum depression. 1 in 1,000 women will develop postpartum psychosis.
“Baby blues” is a slightly antiquated term for the period of adjustment that comes right after baby is born. Mood swings, anxiety and irritability, inability to concentrate, and trouble sleeping can last anywhere from a few days to a few weeks directly postpartum.
However, if these symptoms last longer and/or worsen, it’s possible that postpartum depression has set in (1, 2).

A small percentage of women who bypass baby blues and enter into postpartum depression will experience postpartum psychosis, becoming confused, disoriented, and obsessive, even paranoid in regards to their baby. In extreme cases, this can cause hallucinations, and the mother might feel compelled to harm herself or her baby.
Postpartum psychosis is extremely serious and deserving of direct, immediate attention, however, as I stated above, everyone’s experience is valid and deserves care.
After years of working with women through this phase of life, it caught me off guard that my transition to motherhood was so difficult. Hadn’t I done “all the things” in preparation? There were a lot of instances of me questioning if it was really postpartum depression and anxiety or just that I was sleep deprived and overwhelmed. Overall, I downplayed how bad I really felt for months. It wasn’t until my first was 6 months old that I finally sought the help of a maternal mental health provider at the strong urging of my midwife. By the time I had my second baby, I thought I had prepared even more but found myself struggling worse than with my first for a variety of reasons. Thankfully again, my midwife team and maternal mental health provider were there to help again. What I can see clearly now is that matrascence is a complex transition and while proper nutrition helps provide a foundation, it is not everything! It took me a long time to process that my experiences were not for my lack of preparation or knowledge but a product of many factors that were not at all my fault.
While postpartum depression most directly affects the parent who physically gives birth, partners are not immune to its impact.
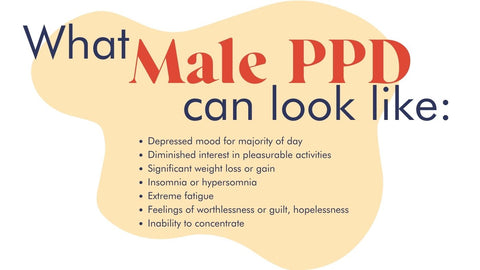
2. Male Postpartum Depression: it's a thing.
On a surface level, it goes without saying that your well being directly correlates to that of your partner’s. Under normal circumstances, we tend to reflect our partner’s moods. When you’re elated, it’s often easy for your significant other to reflect that happiness. Likewise, when you’re feeling stressed, it can easily rub off and consume the energy between the two of you. Add the life-changing element of a new child into the mix and it goes without saying that both of you are wading into uncharted territory. Similar to new moms, a father’s history of depression can impact his mental health during this time, as well as any externally contributing societal factors, such as stress about money, employment, housing, and other familial obligations. Non-birthing partners tend to be focused on the bigger picture of family life and logistics directly after birth, which can be incredibly overwhelming. Sleep deprivation can (let’s be real, it probably will) also wreak havoc on both parents.
However, it’s not always that straightforward when it comes to postpartum depression for men.
Studies show that men also undergo natural hormonal changes during their partner’s pregnancy and for several months following the birth of their child (3). These hormonal shifts are thought to be a sort of evolutionary adaptation to assist the new father in forming a strong bond with his child. Fascinatingly, decreased testosterone levels in new fathers lowers otherwise normal levels of aggression, which in turn increases sympathetic responses to a crying infant. Interesting, right? What’s more, increased estrogen levels in new fathers elevate more paternal parenting behaviors.
So while there are clearly some positive hormonal adjustments that the male body naturally makes after becoming a father, increases in other hormones, like cortisol, the stress hormone, might predispose the father to experience their own form of postpartum depression. That lowered testosterone level can be directly linked to symptoms of depression in men if it goes on for too long.
After the birth of my first, my husband’s needs fell completely by the wayside and were replaced with what baby and I needed. Like so many spouses, he had no paternity leave and was trying to fit in work responsibilities between helping me feed and hydrate myself while breastfeeding our son. He often reflected how helpless he felt in comforting me or our baby given that nursing was all my son wanted to do for comfort for a long time (this is normal but overwhelming!). After our second, again, my husband saw me struggle but also had our toddler demanding any ounce of energy left after other responsibilities. Asking him now how he felt about both postpartum experiences he says, “I felt helpless” and that he also struggled with overwhelm and anxiety about his role and what to do. Particularly, after our second was born which shifted the entire family dynamic again in a big way!
3. Finally, the new baby (and his or her older siblings) can suffer from the PPD that one or both of their parents are going through.
Studies have shown early exposure to excessive stress disrupts the architecture of the developing brain (4). Cues like vocalizations and actions used to communicate with their parents are learned during infancy and into early childhood, but can be disrupted and/or stunted when parents are unintentionally withdrawn for prolonged periods of time. This lack of communication can in turn cause innate fear and undue anxiety for children, which releases chemicals to deal with stress.
The combination of these chemical releases paired with the notion that depressed parents are less likely to offer consistent intellectual stimulation to their infants can have serious developmental consequences. A child’s performance with nonsocial learning tasks can be hindered and the risk of developing emotional disorders increases (5).
"When my daughter was born and we were struggling with the transition, we saw our son regress in a number of ways including our recent successes with potty training and sleeping through the night. We’d been warned that this was normal, and recognized that this transition was also a huge one for him too so despite the frustrations, we did our best to give him the care and attention he needed as well. Ultimately, the worry about how my son was being impacted was the primary driver for me to seek out help quickly after I had my daughter. This still wasn’t easy to do when in the thick of it and is one of the reasons why I always recommend setting up your team of resources before you give birth so that you don’t have to “figure it out” when in the land of overwhelm. I can’t say for sure how my postpartum depression and anxiety affected my son, but he is now a well-adjusted Kindergartener who adores his little sister!"
Remember, help isn’t far away.
Postpartum Support International is one of my favorite organizations that provides a ton of resources for both moms and their families and the health professionals they’ll work with. If you suspect that you or someone you know is suffering from postpartum depression or psychosis, PSI’s directory can help find a provider that specializes in maternal mental health who can immediately assess and help improve the situation.
I love their work so much that Postpartum Support International is part of FullWell’s Giveback Program. We are proud to donate to groups like PSI who do such important work to care for women’s mental health and the well being of their families.
*The information provided on this website is provided for educational purposes only and should not be treated as medical advice. FullWell makes no guarantees regarding the information provided or how products may work for any individual. If you suffer from a health condition, you should consult your health care practitioner for medical advice and before introducing any new products into your health care regimen. For more information please read our terms and conditions.
REFERENCES
1. “Postpartum depression.” The Cleveland Clinic. Web. Accessed September 2021. https://my.clevelandclinic.org/health/diseases/9312-postpartum-depression.
2. “Postpartum depression.” The Mayo Clinic. Web. Accessed September 2021. https://www.mayoclinic.org/diseases-conditions/postpartum-depression/symptoms-causes/syc-20376617.
3. Scarff, Jonathan. “Postpartum Depression in Men.” US National Library of Medicine National Institutes of Health. Web. Published May 2019. Accessed September 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6659987/.
4. “Postpartum Depression Affects More Than Mothers.” The Urban Child Institute. Web. Published October 2013. Accessed September 2021. http://www.urbanchildinstitute.org/articles/perceptions/a-tale-of-two-children-part-5.
5. “Maternal depression and child development.” US National Library of Medicine National Institutes of Health. Web. Published Oct 2004. Accessed September 2021. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2724169/.
This high-protein banana bread is moist, flavorful, and designed to support blood sugar balance. With 20 grams of protein per serving and thoughtful ingredients like almond flour, cottage cheese, and FullWell Collagen Peptides, it’s the perfect nourishing treat for hormone balance, fertility, or simply staying full and energized.*
At a Glance:
Prep time: 15 min | Cook time: 75 min | Yield: 12 muffins
Why This Recipe Supports Blood Sugar Stability & Sustained Energy for Every Stage of Motherhood
Balanced blood sugar is a key part of feeling your best — whether you're preparing your body for conception, navigating the energy swings of pregnancy, or supporting your recovery postpartum. This banana bread is crafted to be more than just a treat:
- High-protein foundation: With 20 grams of protein per slice from FullWell Collagen Peptides, cottage cheese, and egg whites, this recipe supports steady energy, satiety between meals, and recovery — all crucial during pregnancy and postpartum recovery.*
- Naturally sweet with intention: Bananas provide natural sweetness and moisture, while brown sugar is used mindfully to keep the bread satisfying without being overly sugary.
- Smart carbs + healthy fats: Almond flour and chia seeds bring fiber and nourishing fats, helping to slow digestion, support blood sugar regulation, and leave you feeling full and nourished.
Whether you're fighting off morning sickness, managing gestational diabetes, or simply looking for a more balanced way to enjoy banana bread, this recipe has your needs in mind.
Why This Recipe Works in Your Kitchen
The combination of almond flour and FullWell Collagen Peptides can make batters more delicate, but the addition of all-purpose flour, chia seeds, and the structure from egg whites ensures the bread holds together and bakes up with the perfect texture. The long bake time (75 minutes) allows moisture from the bananas and cottage cheese to fully cook off, leaving a dense yet soft loaf that slices beautifully and doesn’t stick to the pan.
Ingredients
- 3-4 medium ripe bananas
- 1 cup cottage cheese (2% low-fat)
- 10 servings liquid egg whites (approx. 30 tbsp or one carton)
- 6 tbsp unsalted butter, melted and cooled
- 2/3 cup brown sugar (unpacked)
- 1 tbsp vanilla extract
- 3 tbsp chia seeds
- 1 cup FullWell Collagen Peptides
- 2½ cups almond flour
- 1 cup all-purpose flour
- ½ tbsp baking soda
- 1 tsp salt
- 1 tsp cinnamon
- ½ tsp ground nutmeg
- Optional add-ins: ½ cup dark chocolate chips or chopped walnuts
Instructions
- Preheat your oven to 350°F, position the oven rack in the middle. Grease a loaf pan with butter and line with parchment paper.
- In a blender, combine bananas, cottage cheese, and egg whites. Blend until smooth (15–20 seconds).
- Pour the banana mixture into a large mixing bowl. Add melted, cooled butter, brown sugar, vanilla extract, and chia seeds. Whisk until smooth.
- In a separate bowl, whisk together almond flour, all-purpose flour, baking soda, salt, cinnamon, nutmeg, and FullWell Collagen Peptides
- Add the dry ingredients to the wet ingredients and mix with a wooden spoon or spatula until just combined. Fold in chocolate chips or nuts if using.
- Pour the batter into the prepared loaf pan, smoothing it evenly.
- Bake for 70–75 minutes, or until the top is golden brown and a toothpick inserted into the center comes out mostly clean with a few moist crumbs.
- Allow the bread to cool completely in the pan before removing and slicing.
Nutrition Facts (per serving)
355 Calories
20 g Protein
28 g Carbs
4 g Fiber
24 g Net Carbs
19 g Fat
Additional Notes
Storage
- Store slices in an airtight container in the refrigerator for up to 5 days. This banana bread also freezes beautifully — slice, wrap, and store in a freezer-safe container for up to 3 months.
Substitutions & Variations
- Cottage cheese: Can be swapped for plain Greek yogurt for a slightly tangier flavor and similar protein content.
- Egg whites: Substitute with 8 whole eggs if desired (to reach the same protein content)
- Brown sugar: Can be replaced with coconut sugar or a monk fruit-brown sugar blend for a lower glycemic option.
- Almond flour: If needed, you can replace it with coconut flour.




